What are varicose veins?
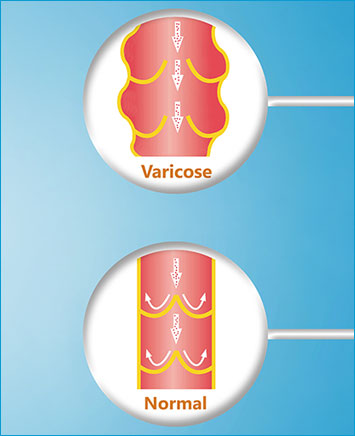
Varicose veins are enlarged, tortuous and superficial veins most commonly found over the front of the thigh, inside of the leg or back of the calf. Any superficial vein can become varicosed but legs are most commonly affected because standing and being in the upright position puts increased pressure on the leg veins which are returning blood to the heart against gravity.
Common, affecting 3 in 10 adults and more likely to develop in women than men, some are simply cosmetic resulting in unsightly lumps which are usually twisted, bulging and purple. More commonly patients experience a number of symptoms including:
- Aching, cramping and heavy legs – particularly towards the end of the day or at night
- Pain and tenderness – especially overlying or on pressing the lumpy veins
- Swelling of the ankles and feet – worse towards the end of the day or prolonged standing
- Itchy, scaly dry skin (varicose eczema)
- Restless legs – again most commonly at night